Abstract
Objectives: To analyze overall survival (OS), leukemia-free survival (LFS), cumulative incidence of relapse (CIR) and non-relapse mortality (NRM) of patients with B cell-acute lymphoblastic leukemia (B-ALL) who received autologous or allogeneic stem cell transplantation and to provide the basis for the choice of transplantation method.
Methods: We retrospectively investigated the outcomes of 388 adult patients with B-ALL in our center. The OS, LFS, CIR and NRM rate and the impact of minimal residual disease (MRD) within 3 chemotherapy cycles along with risk classification were explored.
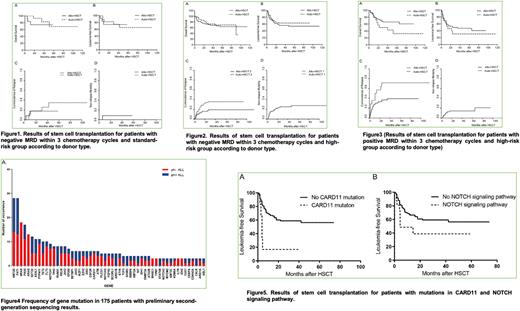
Results: Both univariate and multivariate analysis found that negative MRD within 3 chemotherapy cycles was the important factor associated with the prognosis. As to 355 patients who obtained first complete remission (CR1), we divided patients into 3 groups according to the risk stratification and MRD status within 3 chemotherapy cycles. For patients with negative MRD within 3 chemotherapy cycles and standard-risk group, the 3-year OS (82.5% vs 74.1%, P=0.364), LFS (74.5% vs 74.1%, P=0.904), CIR (25.5% vs 17.6%, P=0.648) and NRM rates(0% vs 8.3%, P=0.234) were not significantly different between autologous hematopoietic stem cell transplantation (auto-HSCT) and allogeneic hematopoietic stem cell transplantation (allo-HSCT) group(Figure 1). In patients with negative MRD and high-risk factors, although auto-HSCT group and allo-HSCT group had similar 3-year OS(72.7% vs 68.5%, P=0.436) and LFS rate (62.8% vs 56.0%, P=0.375) , the lower NRM (1.5% vs 25.1%, P=0.000) was offset by higher CIR(35.7% vs 18.9%, P=0.018) in auto-HSCT group compared with allo-HSCT group(Figure 2). As for other patients with high-risk factors and positive MRD after 3 chemotherapy cycles, the prognosis of auto-HSCT group was evidently worse than those of allo-HSCT group as there was a lower trend of 3-year OS (50.0% vs 66.0%, P=0.077), LFS rate (30.8% vs 47.1%, P=0.398) and significantly higher CIR rate(71.4% vs 39.1%, P=0.018) in auto-HSCT group compared to allo-HSCT group(Figure 3). MRD within 3 chemotherapy cycles was also related to the selection of allogeneic transplantation methods and pretreatment schemes. The 3-year OS (67.4% vs 60.8% vs 65.2%, p=0.735), LFS (56.3% vs 48.3% vs 58.3%, P=0.538), CIR (21.7% vs 23.3% vs 13.3%, P=0.784) and NRM rate (22.1% vs 28.4% vs 28.3%, P=0.672) were similar in matched sibling donor hematopoietic stem cell transplantation (MSD-HSCT), haploid hematopoietic stem cell transplantation (haplo-HSCT) and unrelated donor hematopoietic stem cell transplantation (URD-HSCT) group patients who achieved negative MRD within 3 chemotherapy cycles. While MSD-HSCT group tended to have lower 3-year LFS (33.0% vs 54.1% vs 41.7%, P=0.198) and higher CIR rate (53.2% vs 33.7% vs 46.2%, P=0.233) when comparing with haplo-HSCT and URD-HSCT group patients whose MRD were still positive within 3 chemotherapy cycles. Moreover, in patients who achieved negative MRD within 3 chemotherapy cycles, there was no significant difference in 3-year CIR rate (24.5% vs 23.1%, P=0.784) between TBI group and non-TBI group, but the lower OS (64.2% vs 76.3%, P=0.027) and LFS (54.4% vs 71.3%, P=0.091) was mainly due to the higher NRM rate (17.8% vs 5.6%, P=0.062) in TBI group. For MRD positive patients, TBI group had advantages over non-TBI group, demonstrating a trend of higher 3-year OS (65.0% vs 42.9%, P=0.105), LFS (44.8% vs 27.1%, P=0.138), lower CIR (43.6% vs 63.8%, P=0.106) and similar NRM rate (11.7% vs 9.1%, P=0.671). In addition, we found that 8 most frequently mutated genes were KMT2D、FAT1、NRAS、PAX5、KRAS、SETD2、ASXL1、PTPN11 in 175 patients with preliminary second generation sequencing results(Figure 4). Mutations in CARD11 and NOTCH signaling pathway were correlated with lower LFS (CARD11: 56.3% vs 16.7%, P=0.002; NOTCH signaling pathway: 59.2% vs 38.8%, P=0.049)(Figure 5).
Conclusions: Auto-HSCT with maintenance therapy after HSCT and non-TBI pretreatment schemes appears to be an attractive treatment option for patients with B-ALL especially for those who achieved negative MRD within 3 chemotherapy cycles. For MRD positive patients, allogeneic transplantation and TBI pretreatment schemes may be more effective.
Key words: auto-HSCT, allo-HSCT, acute lymphoblastic leukemia, minimal residual disease
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal